The University is committed to supporting research that may help discover treatments in the fight against COVID-19. CONNECTED looks at how llamas and 3D models are doing just this.
Understanding more about the coronavirus causing the global pandemic is crucial to finding treatments and in developing vaccines. The University is working with scientists in the UK and around the world, from producing llama nanobodies to creating 3D models of the coronavirus, in an effort to better understand the virus and determine potential treatments.
Llamas helping to fight COVID-19
A herd of llamas at the University of Reading are helping UK scientists to find treatments in the fight against COVID-19. The llamas are used to provide nanobodies – very small antibodies – which can be used in a clinical environment to understand how potential  drugs might bind to the SARS-CoV-2 coronavirus.
drugs might bind to the SARS-CoV-2 coronavirus.
The herd, which is looked after by expert handlers at the University of Reading, is being used to produce specialist nanobodies which may be used to block the virus from developing COVID-19 in humans. The nanobodies will be provided to other UK labs, including The Rosalind Franklin Institute and The Francis Crick Institute.
Professor Gary Stephens, from the School of Pharmacy, said:
“Nanobody technology is one of the most exciting new developments in medical research, and llamas play a crucial role in these studies as they are one of the animals from which nanobodies can be produced.
“We’re pleased that the University is using its combined expertise in drug research and animal husbandry to keep a llama herd, and help the scientific effort to develop a treatment for coronavirus.
“A sample of blood from a llama is screened to see whether any of their nanobodies stick to the COVID-19 protein used to generate the response. These can be purified and cloned to generate more identical nanobodies. If we can identify the right antibodies, including nanobodies that will work against coronavirus, we can use these to develop drugs or see if they can stop the virus from reproducing.
“The benefit of using nanobodies produced by llamas is that they may be able to target the virus more effectively and are less prone to being attacked by the human body’s natural defences.
“Demonstrating that llamas can produce unique nanobodies against COVID-19 proteins will be an invaluable tool to aid our understanding of the virus and may lead to the development of a vaccine.”
So far one of Reading’s 15 llamas has been contributing to this work: a 10-year-old female called Fifi, and a further member of the herd will be helping as the study expands. The llamas receive targeted injections a few weeks apart and provide samples of blood to see if they produce antibodies that could work against the coronavirus.
Every injection or blood sample is considered one animal research ‘procedure’, regulated by a government licence and subject to inspection by Home Office expert officials, and is counted in the University’s annual reported animal research statistics. Such procedures are considered ‘mild’ on a scale of severity to the animal.
Professor Ray Owens, who leads Protein Production UK for The Rosalind Franklin Institute, said:
“There is an unprecedented level of teamwork and collaboration globally to image, understand, and treat COVID-19. We are working with colleagues at the University of Reading and Oxford to develop a pipeline for nanobodies to gain insights into the structure of the virus that causes COVID-19.”
Svend Kjaer, Deputy of the Structural Biology Science Technology Platform at The Francis Crick Institute said:
“The collaboration with the University’s llama facility is a great opportunity for the Crick Institute to generate sustainable supplies of versatile, high-value nanobodies for multiple applications in ongoing COVID-19 research programmes.”
3D models bring coronavirus into view
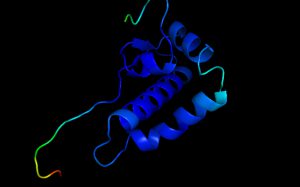 While Fifi the llama is busy helping to discover treatments for COVID-19, Reading’s Dr Liam McGuffin is also working hard to help the scientific community understand how to combat the virus with new or existing drugs. Dr McGuffin is part of an international team producing detailed 3D models of important proteins of the coronavirus, contributing to the efforts of the CASP Commons 2020 programme.
While Fifi the llama is busy helping to discover treatments for COVID-19, Reading’s Dr Liam McGuffin is also working hard to help the scientific community understand how to combat the virus with new or existing drugs. Dr McGuffin is part of an international team producing detailed 3D models of important proteins of the coronavirus, contributing to the efforts of the CASP Commons 2020 programme.
Dr McGuffin, Associate Professor in Bioinformatics in the School of Biological Sciences, said:
“The coronavirus has been called an invisible killer. Our work helps to lift the cloak of invisibility, providing a clearer view of the virus, and helping show how we can fight it.
“Viruses are so tiny that it is very hard to know what they look like, or how they work, just by looking at them, even with powerful microscopes. Modelling the virus proteins is like breaking it down into its constituent parts and then putting it back together again to show how it works.”
The scientific group of 52 research teams across the world has already created 1,600 3D models of parts of the SARS-CoV-2 coronavirus. The 3D digital models can be used by scientists trying to find out more about the protein-based ‘building blocks’ of the coronavirus, which can help show what it looks like; what each part of the virus does; and how different parts interact with each other, and with human cells.
This information could be vital to scientists looking to see which existing or new drugs might combat the virus, and for those developing vaccines.
Dr McGuffin said the modellers were showing what was going on beneath the surface of the virus:
“The outside of the coronavirus is quite well characterised structurally, but many of the proteins we want to understand are hidden away from the surface.
“These proteins are used by the virus at important points in its life cycle, as it enters human cells and replicates itself.
“We have focused on modelling parts of the virus that we knew the least about. The aim is to shine a light on these unknown proteins, for which there is little experimental data, by using cutting-edge artificial intelligence and deep learning methods to build up a detailed picture of the coronavirus, and how it works.”
Discover more about the University of Reading’s research in the fight against COVID-19.